Hearing Loss
Types of Hearing Loss
There are three main types of hearing loss: conductive hearing loss, sensorineural hearing loss, and mixed hearing loss.
Conductive hearing loss occurs when there is a problem with the outer or middle ear, which prevents sound from being transmitted properly to the inner ear. This type of hearing loss can be caused by earwax buildup, fluid in the ear, a punctured eardrum, or a structural problem with the ear.
Sensorineural hearing loss occurs when there is damage to the inner ear or the nerve pathways that transmit sound to the brain. This type of hearing loss is usually permanent and can be caused by aging, genetics, exposure to loud noises, illness, or injury.
Mixed hearing loss is a combination of conductive and sensorineural hearing loss.
Prevalence of Hearing Loss
Hearing loss is a common condition that affects millions of people around the world. According to the World Health Organization (WHO), approximately 466 million people worldwide have disabling hearing loss, and this number is projected to increase to over 900 million by 2050. Hearing loss can occur at any age, but it is most commonly diagnosed in older adults.
Causes of Hearing Loss
There are many potential causes of hearing loss, including:
- Exposure to loud noises: Prolonged exposure to loud noises can damage the hair cells in the inner ear and cause permanent hearing loss.
- Aging: Hearing loss is a common part of the aging process, and it is estimated that one in three people over the age of 65 experience some degree of hearing loss.
- Genetics: Some people are born with genetic conditions that cause hearing loss.
- Illness: Certain illnesses, such as meningitis, measles, and mumps, can cause hearing loss.
- Injury: Head injuries or trauma to the ear can cause hearing loss.
- Medications: Certain medications, such as certain antibiotics and chemotherapy drugs, can cause hearing loss as a side effect.
Symptoms of Hearing Loss
The symptoms of hearing loss can vary depending on the type and severity of the hearing loss. Some common symptoms of hearing loss include:
- Difficulty hearing conversations in noisy environments
- Trouble understanding speech, especially when there is background noise
- Asking people to repeat themselves frequently
- Turning up the volume on the TV or radio to levels that others find uncomfortable
- Avoiding social situations because of difficulty hearing
Treatment for Hearing Loss
The treatment for hearing loss depends on the type and severity of the hearing loss. Some common treatments for hearing loss include:
- Hearing aids: Hearing aids are electronic devices that amplify sound and help people with hearing loss hear better. There are many different types of hearing aids available, including behind-the-ear (BTE) models, in-the-ear (ITE) models, and completely-in-canal (CIC) models.
- Cochlear implants: Cochlear implants are devices that are surgically implanted in the inner ear and can help people with severe-to-profound hearing loss hear better. Cochlear implants work by bypassing the damaged hair cells in the inner ear and stimulating the auditory nerve directly.
- Assistive listening devices: Assistive listening devices (ALDs) are devices that help people with hearing loss hear better in specific situations. ALDs can be used in conjunction with hearing aids or alone and can be helpful in situations such as watching TV or listening to lectures.
- Communication strategies: People with hearing loss can also benefit from learning communication strategies such as lip reading, using visual cues, and positioning themselves appropriately in relation to the speaker.
Hearing Loss and Cognitive Decline
Hearing loss and cognitive decline are two distinct phenomena that have been found to be interconnected in recent years. Hearing loss refers to the diminished ability to perceive and process sound, while cognitive decline refers to a gradual deterioration in cognitive abilities such as memory, attention, and problem-solving skills. In this essay, we will explore the relationship between hearing loss and cognitive decline, the possible causes, and potential interventions.
Causes of Hearing Loss and Cognitive Decline
Hearing loss can result from various factors, including age-related changes, exposure to loud noise, certain medications, and genetic factors. As people age, the structures within the ear responsible for transmitting sound signals may deteriorate, leading to reduced auditory function. Prolonged exposure to loud noises can damage the hair cells within the inner ear, which are essential for converting sound vibrations into electrical signals that the brain can interpret. Some medications, such as chemotherapy drugs and certain antibiotics, can also cause temporary or permanent hearing loss. Finally, genetics can play a role in determining an individual’s susceptibility to hearing loss.
Cognitive decline, on the other hand, can result from various factors including aging, neurological disorders, and lifestyle choices. Age-related cognitive decline is a natural process that occurs as the brain’s structure and function change over time. Neurological disorders, such as Alzheimer’s disease and Parkinson’s disease, can also contribute to cognitive decline. Lifestyle factors, including physical activity, diet, and social engagement, can also influence cognitive health.
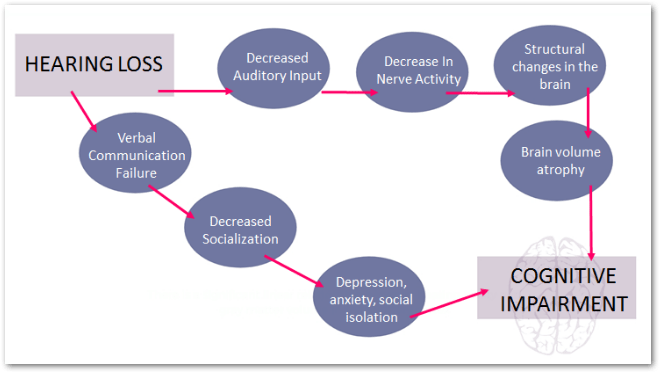
The Connection Between Hearing Loss and Cognitive Decline
Research has shown that there is a significant association between hearing loss and cognitive decline. Studies have found that individuals with hearing loss are more likely to experience accelerated cognitive decline and are at an increased risk of developing dementia. This connection may be due to several factors:
- Cognitive Overload: When someone experiences hearing loss, their brain has to work harder to process and understand speech, which can lead to cognitive overload. This constant strain on the brain may contribute to cognitive decline over time.
- Social Isolation: Untreated hearing loss can lead to social isolation, as individuals may avoid situations where communication is difficult or stressful. Social isolation has been linked to an increased risk of cognitive decline and dementia.
- Increased Brain Atrophy: Research has shown that individuals with hearing loss exhibit greater rates of brain atrophy, particularly in areas associated with auditory processing and memory. This atrophy may contribute to cognitive decline over time.
Interventions for Hearing Loss and Cognitive Decline
Given the strong association between hearing loss and cognitive decline, addressing hearing loss may be an essential step in promoting cognitive health. Some potential interventions include:
- Hearing Aids: Wearing hearing aids can help improve auditory function and reduce cognitive overload. Studies have shown that using hearing aids can slow down the rate of cognitive decline in older adults with hearing loss.
- Cognitive Training: Engaging in regular cognitive training exercises, such as puzzles, memory games, and social activities, can help maintain and improve cognitive function.
- Lifestyle Modifications: Adopting a healthy lifestyle, including regular physical exercise, a balanced diet, and maintaining strong social connections, can contribute to better overall cognitive health.
What is Ménière’s disease?
Ménière’s disease is an inner ear disorder that affects the balance and hearing. It is named after the French physician Prosper Ménière, who first described the condition in 1861. The disease is characterized by episodes of vertigo, tinnitus, hearing loss, and a feeling of fullness in the affected ear.
Symptoms of Ménière’s Disease
The primary symptoms of Ménière’s disease are:
- Vertigo: A spinning sensation that can last from minutes to hours. It is often accompanied by nausea and vomiting.
- Tinnitus: A ringing, buzzing, or roaring sound in the affected ear.
- Hearing Loss: A sensorineural hearing loss that can fluctuate and may become permanent over time.
- Aural Fullness: A feeling of pressure or fullness in the affected ear.
These symptoms can occur separately or in combination, and their severity can vary from person to person.
Causes of Ménière’s Disease
The exact cause of Ménière’s disease is not known, but it is believed to be related to an abnormal amount of fluid (endolymph) in the inner ear. This fluid buildup can disrupt the normal functioning of the inner ear, leading to the symptoms of Ménière’s disease. Factors that may contribute to this fluid buildup include genetics, autoimmune disorders, viral infections, and allergies.
Diagnosis of Ménière’s Disease
There is no definitive test for Ménière’s disease. The diagnosis is typically made based on the patient’s symptoms, a physical examination, and a series of tests to rule out other conditions. These tests may include hearing tests, balance tests, and imaging studies like MRI or CT scans.
Treatment of Ménière’s Disease
There is no cure for Ménière’s disease, but various treatments can help manage the symptoms:
- Dietary Changes: Avoiding salt, caffeine, and alcohol can help reduce the severity and frequency of symptoms.
- Diuretics: Medications that help reduce the amount of fluid in the inner ear may be prescribed.
- Vestibular Rehabilitation: Physical therapy exercises can help improve balance and reduce dizziness.
- Anti-Vertigo Medications: Medications like meclizine or diazepam can help relieve vertigo.
- Steroids: Corticosteroids can reduce inflammation and swelling in the inner ear.
- Surgery: In severe cases, surgery may be recommended to treat or prevent further damage to the inner ear.
Living with Ménière’s Disease
Living with Ménière’s disease can be challenging due to its unpredictable nature. However, with appropriate treatment and lifestyle changes, many people with Ménière’s disease are able to manage their symptoms and maintain a good quality of life. Support groups and counseling can also be helpful for individuals dealing with the emotional impact of this condition.
The Hearing System: How It Works
Sound Waves Reception: When sound waves enter the ear, they travel through the ear canal and reach the eardrum. The eardrum vibrates in response to the sound waves.
Middle Ear Transmission: The vibrations from the eardrum are then transmitted through three small bones in the middle ear called the ossicles – the malleus, incus, and stapes. These bones amplify the vibrations and transmit them to the inner ear.
Inner Ear Processing: In the inner ear, the cochlea is a spiral-shaped organ filled with fluid. As the vibrations reach the cochlea, they cause tiny hair cells to move. These hair cells convert the vibrations into electrical signals that are sent to the brain through the auditory nerve.
Brain Interpretation: The auditory nerve carries these electrical signals to the brain, specifically to the auditory cortex in the temporal lobe. The brain processes these signals and interprets them as sound, allowing us to perceive and understand what we hear.
Will Hearing Deteriorate Without Wearing a Hearing Aid?
Hearing aids are devices designed to amplify sounds for individuals with hearing loss. The decision to wear a hearing aid is often based on the severity of the hearing loss and the individual’s lifestyle needs. While wearing a hearing aid can significantly improve communication and quality of life for those with hearing impairment, the question of whether not wearing a hearing aid will lead to further deterioration in hearing is a common concern.
Effects of Not Wearing a Hearing Aid
- Social Isolation: One of the primary consequences of untreated hearing loss is social isolation. Difficulty in understanding conversations can lead to withdrawal from social interactions, which can impact mental health and overall well-being.
- Auditory Deprivation: Auditory deprivation refers to the concept that when the auditory system is not stimulated adequately, it may lead to a decline in speech understanding over time. This means that without the use of a hearing aid, the brain may lose its ability to process sounds effectively.
- Cognitive Decline: Research has shown a link between untreated hearing loss and cognitive decline. Straining to hear and understand conversations can put additional cognitive load on the brain, potentially contributing to conditions like dementia.
- Increased Risk of Falls: Hearing loss has been associated with an increased risk of falls, especially in older adults. Not being able to hear environmental cues or warnings can lead to accidents and falls.
- Tinnitus: For some individuals with untreated hearing loss, tinnitus (ringing in the ears) may become more pronounced. Tinnitus can be distressing and impact quality of life.
Preventing Further Hearing Deterioration
While not wearing a hearing aid may not directly cause additional deterioration in hearing, it can exacerbate existing issues and lead to various negative consequences as mentioned above. To prevent further deterioration and maintain overall well-being, it is essential for individuals with hearing loss to consider using appropriate interventions such as hearing aids, assistive listening devices, or other treatments recommended by healthcare professionals.
In conclusion, while not wearing a hearing aid may not directly cause irreversible damage to one’s hearing, it can have significant negative effects on communication, social interactions, cognitive function, and overall quality of life. Seeking appropriate interventions and support for hearing loss is crucial in managing the condition effectively.
Ear Pathology
An ear pathology refers to any abnormal condition or disease affecting the ear. This can include issues with the outer ear, middle ear, inner ear, or a combination of these areas. Ear pathologies can be caused by various factors such as infections, trauma, genetic disorders, autoimmune diseases, or exposure to loud noises. Common ear pathologies include otitis media (middle ear infection), otosclerosis (abnormal bone growth in the middle ear), Meniere’s disease (inner ear disorder affecting balance and hearing), and tinnitus (ringing in the ears). Proper diagnosis and treatment of ear pathologies are essential to prevent complications and preserve hearing function.
Causes of Ear Pathologies
Ear pathologies can have various causes, including:
- Infections: Bacterial or viral infections can affect different parts of the ear, leading to conditions like otitis externa (outer ear infection) or otitis media (middle ear infection).
- Trauma: Injuries to the ear from accidents, loud noises, or foreign objects can result in ear pathologies.
- Genetic Disorders: Some individuals may inherit genetic conditions that predispose them to certain ear pathologies.
- Autoimmune Diseases: Conditions like autoimmune inner ear disease can cause inflammation and damage to the structures of the ear.
- Exposure to Loud Noises: Prolonged exposure to loud noises can lead to hearing loss and other ear pathologies.
Symptoms of Ear Pathologies
The symptoms of an ear pathology can vary depending on the specific condition but may include:
- Pain or discomfort in the ear
- Hearing loss or changes in hearing
- Tinnitus (ringing in the ears)
- Dizziness or vertigo
- Ear drainage or discharge
- Itching or irritation in the ear
Diagnosis and Treatment
Diagnosis of an ear pathology typically involves a thorough medical history, physical examination, and may include tests such as audiometry, tympanometry, imaging studies like CT scans or MRI, and blood tests. Treatment options for ear pathologies depend on the underlying cause and may include medications (such as antibiotics for infections), hearing aids, surgery (e.g., for otosclerosis), or lifestyle modifications.
Will Wearing a Hearing Aid Damage My Hearing?
No, wearing a hearing aid properly will not damage your hearing.
How Hearing Aids Work: Hearing aids are designed to amplify sounds for individuals with hearing loss. They do not emit any harmful radiation or sound that could damage your hearing when used correctly. The purpose of a hearing aid is to help individuals hear better by making sounds louder and clearer, but they are specifically calibrated to ensure they do not exceed safe levels for the user.
Proper Usage of Hearing Aids: It is crucial to use hearing aids as prescribed by an audiologist or hearing healthcare professional. Following their guidance on the fitting, volume adjustment, and maintenance of the device is essential to prevent any potential harm to your hearing. Using a hearing aid at the appropriate volume levels and for the recommended duration will not cause damage to your ears.
Benefits of Hearing Aids: Wearing a hearing aid can significantly improve your quality of life by enhancing your ability to communicate, engage in conversations, and participate in various activities. By providing access to sounds that were previously difficult to hear, hearing aids can help prevent social isolation and cognitive decline associated with untreated hearing loss.
In conclusion, wearing a hearing aid correctly will not damage your hearing. It is essential to consult with a professional for proper fitting and usage instructions to ensure the device effectively improves your hearing without causing any harm.
What is a Hearing Test
A hearing test, also known as an audiometry or audiologic evaluation, is a series of tests that are conducted to evaluate the sensitivity of a person’s sense of hearing. These tests are typically performed by audiologists, healthcare professionals who specialize in diagnosing and treating hearing disorders.
During a hearing test, various methods may be used to assess different aspects of hearing, including:
- Pure-tone audiometry: This test involves listening to tones at different frequencies and volumes through headphones. The individual indicates when they can hear the tones, which helps determine the softest sounds they can detect at various frequencies.
- Speech audiometry: This test evaluates how well a person can understand speech at different volumes. It may involve repeating words or sentences presented at varying levels of loudness.
- Tympanometry: This test assesses the health and function of the middle ear by measuring how the eardrum responds to changes in air pressure.
Hearing tests are essential for identifying hearing loss, determining its type and severity, and developing appropriate treatment plans, such as hearing aids or cochlear implants. They are also crucial for monitoring changes in hearing over time and assessing the effectiveness of interventions.
In summary, a hearing test is a comprehensive evaluation of an individual’s ability to hear sounds across different frequencies and volumes, using various tests to assess different aspects of their auditory system.
Types of Ear Injuries
- Traumatic Ear Injuries: Trauma to the ear can occur due to direct blows, falls, or accidents. This type of injury may result in a ruptured eardrum (tympanic membrane perforation), which can cause pain, hearing loss, and sometimes bleeding from the ear. Treatment for traumatic ear injuries may involve rest, antibiotics to prevent infection, and in severe cases, surgical repair of the eardrum.
- Acoustic Trauma: Exposure to loud noises, such as explosions or loud machinery, can cause damage to the delicate structures of the inner ear. Acoustic trauma can lead to sensorineural hearing loss, tinnitus, and a feeling of fullness in the ear. Prevention of acoustic trauma involves using ear protection in noisy environments and limiting exposure to loud sounds.
- Barotrauma: Changes in air pressure, such as during air travel or scuba diving, can result in barotrauma to the ear. This condition may cause pain, a feeling of pressure in the ears, dizziness, and hearing loss. To prevent barotrauma, techniques like swallowing, yawning, or using specialized earplugs can help equalize pressure during altitude changes.
- Foreign Body Injuries: Inserting foreign objects into the ear canal can lead to injuries or blockages. Common foreign bodies include cotton swabs, small toys, or insects. Attempting to remove foreign objects from the ear without professional assistance can worsen the injury or push the object deeper into the ear canal. Seeking medical attention is crucial for safe removal and treatment.
- Infectious Ear Injuries: Infections of the outer ear (otitis externa) or middle ear (otitis media) can cause pain, swelling, discharge from the ear, and sometimes fever. These infections are often treated with antibiotics or antifungal medications depending on the underlying cause. Chronic or recurrent infections may require further evaluation by an otolaryngologist.
Treatment and Management
The treatment for ear injuries varies depending on the type and severity of the injury. It is essential to seek medical attention if you experience persistent pain, bleeding from the ear, sudden hearing loss, or any other concerning symptoms related to your ears. Avoid self-diagnosis and self-treatment when it comes to ear injuries to prevent complications and ensure proper care.
In conclusion, understanding the different types of ear injuries and their respective treatments is crucial for maintaining ear health and preventing long-term complications. By taking preventive measures and seeking timely medical intervention when needed, individuals can protect their ears from potential harm and preserve their hearing abilities.
Sudden Hearing Loss? What To Do
Immediate Steps to Take
- Seek Medical Attention: The sudden loss of hearing, also known as sudden sensorineural hearing loss, requires immediate medical attention. Contact an ear, nose, and throat (ENT) specialist or visit the emergency room as soon as possible.
- Avoid Self-Diagnosis: Refrain from attempting to self-diagnose or self-medicate. Sudden hearing loss can have various causes, including infections, blockages, or more serious underlying conditions that require professional evaluation.
- Keep Calm: While experiencing sudden hearing loss can be distressing, it is essential to remain calm and seek prompt medical assistance.
Medical Evaluation and Treatment
Upon seeking medical attention for sudden hearing loss, the healthcare provider may conduct a thorough evaluation to determine the underlying cause. This evaluation may include:
- Physical Examination: The healthcare provider will examine your ears and may assess your overall health to identify any potential contributing factors.
- Hearing Tests: Audiometric tests such as pure-tone audiometry and speech audiometry may be conducted to assess the extent and nature of the hearing loss.
- Imaging Studies: In some cases, imaging studies such as MRI or CT scans may be recommended to rule out structural issues within the ear or surrounding areas.
Possible Causes of Sudden Hearing Loss
Sudden sensorineural hearing loss can have various causes, including:
- Viral Infections: Conditions such as viral infections affecting the inner ear, like vestibular neuritis or viral labyrinthitis, can lead to sudden hearing loss.
- Vascular Issues: Problems related to blood circulation in the inner ear, such as microvascular ischemia, can result in sudden sensorineural hearing loss.
- Autoimmune Disorders: Conditions like autoimmune inner ear disease (AIED) can cause sudden hearing loss due to the immune system attacking the inner ear structures.
Recovery and Rehabilitation
The prognosis for sudden hearing loss varies depending on the underlying cause and promptness of treatment. Some individuals may experience partial or complete recovery of their hearing with appropriate interventions. Rehabilitation options such as hearing aids or assistive devices may be recommended if permanent hearing loss occurs.
It is crucial to follow the guidance of healthcare professionals and attend follow-up appointments to monitor progress and adjust treatment plans accordingly.
Is Hearing Loss Hereditary?
Yes, hearing loss can be hereditary.
Genetic Factors in Hearing Loss: Hearing loss can be caused by genetic factors that are passed down from parents to their children. There are several genetic conditions that can lead to hearing loss, such as:
- Autosomal Dominant Hearing Loss: In this type of inheritance pattern, a mutation in one copy of the gene is sufficient to cause hearing loss. Examples of autosomal dominant genetic hearing loss include DFNA2 and DFNA9.
- Autosomal Recessive Hearing Loss: Autosomal recessive inheritance requires both copies of the gene to have mutations for the individual to experience hearing loss. Examples of autosomal recessive genetic hearing loss include DFNB1 and DFNB9.
- Mitochondrial Inheritance: Some forms of genetic hearing loss are inherited through mitochondrial DNA, which is passed down from the mother to her offspring. Mitochondrial inheritance patterns can lead to conditions like maternally inherited deafness.
- X-Linked Hearing Loss: This type of inheritance involves genes located on the X chromosome. X-linked hearing loss can affect males more severely than females due to males having only one X chromosome.
Environmental Factors in Hearing Loss: While genetic factors play a significant role in hereditary hearing loss, it’s essential to note that environmental factors can also contribute to hearing impairment. Exposure to loud noises, ototoxic medications, infections, and aging can all lead to acquired hearing loss, which is not directly linked to genetics.
In conclusion, while some forms of hearing loss are hereditary and can be passed down through generations due to genetic mutations, other types of hearing loss may result from environmental factors or a combination of genetic and environmental influences.
Will Wearing Hearing Aids Make My Hearing Worse?
No, wearing hearing aids will not make your hearing worse.
How Hearing Aids Work: Hearing aids are designed to amplify sounds and help individuals with hearing loss hear better. They do not cause or worsen hearing loss. In fact, wearing hearing aids can actually prevent auditory deprivation, which is the deterioration of the auditory system due to lack of stimulation.
Benefits of Hearing Aids:
- Improved communication: Hearing aids can help individuals hear conversations more clearly, making it easier to communicate with others.
- Enhanced quality of life: By improving hearing ability, hearing aids can enhance overall quality of life by allowing individuals to engage more fully in social activities and daily interactions.
- Prevention of cognitive decline: Studies have shown that untreated hearing loss can be linked to cognitive decline, while wearing hearing aids can help maintain cognitive function.
Proper Use of Hearing Aids: It is important to use hearing aids as prescribed by a qualified Audiometrist, Audiologist or hearing healthcare professional. Proper fitting and regular maintenance are essential for optimal performance and to prevent any potential issues.
In conclusion, wearing hearing aids will not make your hearing worse; in fact, they can significantly improve your ability to hear and communicate effectively.
Will Hearing Loss Deteriorate Without Wearing Hearing Aids?
Hearing loss can indeed deteriorate if left untreated by not wearing hearing aids. The use of hearing aids is crucial in managing and potentially slowing down the progression of hearing loss. When a person with hearing loss does not wear hearing aids, they are more likely to experience further deterioration in their ability to hear and understand speech over time.
Impact of Untreated Hearing Loss:
- Social Isolation: Without the assistance of hearing aids, individuals may struggle to communicate effectively in social settings, leading to feelings of isolation and withdrawal from social interactions.
- Cognitive Decline: Research has shown a link between untreated hearing loss and cognitive decline, including an increased risk of conditions like dementia. By not wearing hearing aids, individuals may be at a higher risk of experiencing cognitive challenges.
- Emotional Well-being: Untreated hearing loss can also impact emotional well-being, leading to feelings of frustration, anxiety, and depression due to difficulties in communication and understanding.
Progression of Hearing Loss:
Hearing loss is often progressive, meaning it can worsen over time if left untreated. By not using hearing aids, individuals may strain to hear sounds and conversations, causing further damage to their auditory system. This can result in a decline in overall hearing ability and make it more challenging to benefit from interventions later on.
Prevention and Management:
Wearing hearing aids can help individuals with hearing loss maintain their auditory stimulation, improve communication abilities, and preserve their overall quality of life. Regular check-ups with an Audiometrist or Audiologist can also ensure that the hearing aids are appropriately adjusted to meet the individual’s changing needs.
In conclusion, not wearing hearing aids when experiencing hearing loss can lead to the deterioration of one’s ability to hear and understand sounds. It is essential to seek professional guidance and utilize appropriate interventions like hearing aids to manage and potentially slow down the progression of hearing loss.
What is Benign Paroxysmal Positional Vertigo (BPPV)
Benign Paroxysmal Positional Vertigo (BPPV) is a common disorder of the inner ear characterized by brief episodes of dizziness triggered by changes in head position. It is considered benign because it is not life-threatening and usually resolves on its own or with simple treatments.
Symptoms:
- The primary symptom of BPPV is a sudden sensation of spinning or vertigo that occurs with certain head movements, such as rolling over in bed, looking up, or bending over.
- Some individuals may also experience nausea, vomiting, imbalance, and lightheadedness during an episode of BPPV.
Causes:
- BPPV is typically caused by the displacement of small calcium carbonate crystals (otoconia) within the inner ear’s semicircular canals. These crystals can disrupt the normal flow of fluid in the canals, leading to false signals being sent to the brain about head position and movement.
Diagnosis:
- Diagnosis of BPPV is usually based on an individuals medical history and physical examination, including specific positional tests like the Dix-Hallpike manoeuvre or the supine roll test.
- Additional tests such as electronystagmography (ENG) or videonystagmography (VNG) may be used to confirm the diagnosis and rule out other potential causes of vertigo.
Treatment:
- The Epley manoeuvre is a common treatment for BPPV that involves a series of head movements to reposition the displaced crystals within the inner ear.
- Brandt-Daroff exercises and Semont-Liberatory maneuvers are other techniques that can help alleviate symptoms and reposition the otoconia.
- In some cases, medications like vestibular suppressants or anti-nausea drugs may be prescribed to manage symptoms during episodes of vertigo.
Prognosis:
- BPPV is generally a self-limiting condition that tends to improve over time, with many individuals experiencing resolution of symptoms within a few weeks to months.
- Recurrence of BPPV is possible, but repeated treatments are usually effective in managing symptoms and preventing future episodes.
Prevention:
There are no specific preventive measures for BPPV, but avoiding sudden head movements or maintaining good head positioning during activities that trigger symptoms may help reduce the risk of episodes.
Osteoporosis/Osteopenia and Hearing Loss
Osteoporosis and hearing loss are two common health issues, especially in the aging population. While they may seem unrelated, recent studies have suggested a potential link between osteoporosis and hearing loss. This answer will explore the relationship between osteopenia and hearing loss, focusing on the most authoritative and popular internet sources.
Osteopenia and Osteoporosis: An Overview
Osteopenia is a condition characterized by decreased bone density, which is not as severe as osteoporosis. It is often considered a precursor to osteoporosis, a more serious condition that weakens bones and makes them more prone to fractures. Both osteopenia and osteoporosis are caused by a decrease in bone mass and density over time, which can be influenced by factors such as aging, genetics, lifestyle, and hormonal changes.
Hearing Loss: Types and Causes
Hearing loss can be classified into two main types: conductive hearing loss and sensorineural hearing loss. Conductive hearing loss occurs when there is a problem with the outer or middle ear, preventing sound from reaching the inner ear. Sensorineural hearing loss, on the other hand, is caused by damage to the inner ear or the nerve pathways from the inner ear to the brain. This type of hearing loss is more common and often permanent.
Causes of hearing loss can include exposure to loud noises, ear infections, genetics, aging, and certain medical conditions. Hearing loss can also be a side effect of some medications.
The Link Between Osteoporosis/Osteopenia and Hearing Loss
Several studies have suggested a potential link between osteoporosis/osteopenia and hearing loss. One study published in the Journal of Clinical Endocrinology & Metabolism found that women with osteoporosis had a higher risk of developing hearing loss than those without osteoporosis. Another study published in the Journal of the American Geriatrics Society found that men with low bone density were more likely to have hearing loss than those with normal bone density.
The exact mechanism behind this link is not fully understood, but it is believed that there may be a common factor that contributes to both conditions, such as aging or inflammation. Additionally, some researchers suggest that the structural changes in the bones of the inner ear may be similar to those seen in osteoporosis/osteopenia, which could contribute to hearing loss.
Prevention and Treatment
While more research is needed to fully understand the relationship between osteoporosis/osteopenia and hearing loss, there are steps that can be taken to prevent or manage both conditions. These include:
- Regular exercise to maintain bone density and overall health
- A healthy diet rich in calcium and vitamin D to support bone health
- Avoiding smoking and excessive alcohol consumption
- Protecting ears from loud noises by wearing earplugs or avoiding noisy environments
- Regular hearing tests to detect any changes in hearing ability early on
- Medications or supplements to manage osteoporosis/osteopenia or hearing loss, if necessary.
Conclusion
In conclusion, there appears to be a potential link between osteoporosis/osteopenia and hearing loss. While more research is needed to fully understand this relationship, maintaining a healthy lifestyle through regular exercise, a balanced diet, avoiding harmful habits, and regular check-ups can help prevent or manage both conditions. If you are concerned about your bone density or hearing ability, it is recommended to consult with a healthcare professional for further evaluation and advice.
What is Auditory Deprivation?
Auditory deprivation occurs when the brain is deprived of sound, typically due to untreated hearing loss. Over time, this lack of auditory stimulation leads to a decline in the brain’s ability to process sound. If left untreated, the parts of the brain responsible for hearing can undergo atrophy or shrinkage as they are not being used for their intended function. This phenomenon can affect individuals with varying degrees of hearing loss, not just those with severe impairment.
Brain Atrophy from Untreated Hearing Loss
When hearing loss is left untreated, the brain adapts to the reduced input of sound signals by reallocating resources. Even minor hearing loss can cause changes in how the brain processes information, potentially shifting from auditory to visual processing. The longer hearing loss remains untreated, the more likely it is that the auditory parts of the brain may be repurposed for other functions. This can make it challenging to effectively treat hearing loss even after using hearing aids.
Use It or Lose It: Hearing Loss and Brain Function
Audiometrists and Audiologists emphasize the importance of addressing hearing loss promptly with the phrase “use it or lose it.” Delaying treatment can lead to difficulties in understanding and processing information as the brain struggles to interpret sounds correctly. The longer the delay in seeking treatment, the more challenging it may become for the brain to process auditory information accurately.
Is Auditory Deprivation Permanent?
The permanence of cerebral atrophy resulting from auditory deprivation varies among individuals. While it is uncertain whether these changes are permanent, research suggests that consistent use of hearing aids may help reverse some negative adaptations in the brain. The brain’s plasticity allows for potential improvements in processing sound signals and may slow down or halt further brain shrinkage over time.
Cognitive Load and Hearing Loss
Cognitive Load: Cognitive load refers to the amount of mental effort or resources required to perform a particular task. It is the burden placed on a person’s cognitive system when processing information, making decisions, or solving problems. When the cognitive load exceeds an individual’s mental capacity, it can lead to cognitive overload, where the demands on the person’s mental work surpass their abilities to cope effectively.
Hearing Loss and Cognitive Load: Hearing loss can significantly impact cognitive load due to the challenges individuals with hearing impairment face in processing auditory information. When someone has difficulty hearing, especially in noisy environments or when trying to focus on a conversation, they may experience increased cognitive load as they expend more mental effort to understand speech and fill in missing information. This additional cognitive effort can lead to fatigue, reduced comprehension, and overall cognitive strain.
Connection Between Hearing Loss and Cognitive Overload:
- Impact on Brain Activity: Studies have shown that individuals with hearing loss may exhibit altered brain activity patterns compared to those with normal hearing. The brain of a person with hearing impairment may compensate for the deficits in sound processing by recruiting additional neural resources related to language comprehension. This recruitment of extra brain areas for auditory tasks can contribute to cognitive overload as the brain works harder to interpret and make sense of sounds.
- Reduced Activation in Sound Processing Areas: Functional MRI studies have demonstrated that people with poor hearing exhibit reduced activation in brain regions responsible for sound processing. This decreased activation in primary auditory areas suggests that individuals with hearing loss may struggle more with basic auditory tasks, leading to compensatory mechanisms that involve other brain regions associated with language processing.
- Strategies to Reduce Cognitive Load: Individuals with hearing loss can employ various strategies to reduce cognitive load and enhance communication efficiency. These strategies include using visual cues, reducing background noise, utilizing assistive devices like hearing aids or cochlear implants, practicing active listening techniques, and engaging in activities that promote relaxation and focus.
In summary, hearing loss can contribute to cognitive overload by increasing the mental effort required for auditory processing and comprehension. Understanding the connection between hearing loss and cognitive load is essential for developing effective interventions and support strategies for individuals experiencing both conditions.
Can Headphones Cause Hearing Loss?
Yes, overexposure to headphones can damage your hearing.
Hearing Loss Due to Headphones
Listening to loud music through headphones or earbuds for extended periods can lead to noise-induced hearing loss. The prolonged exposure to high volumes can cause damage to the auditory nerve and the delicate hair cells in the inner ear, resulting in temporary or permanent hearing loss.
Signs of Hearing Loss
Some common warning signs of hearing loss due to headphone use include:
- Muffled sounds
- Difficulty understanding conversations in noisy environments
- Trouble hearing high-pitched sounds
- Struggling with speech consonants
- Ringing in the ears (tinnitus)
- Asking others to repeat themselves or speak louder
- Hypersensitivity to certain sounds
Prevention of Hearing Loss with Headphones
To prevent hearing damage while using headphones, consider the following measures:
- Limit Volume: Keep the volume at a moderate level, not exceeding 60% of the maximum volume.
- Limit Duration: Avoid prolonged listening sessions; adhere to the 60/60 rule – no more than 60% volume for a maximum of 60 minutes per day.
- Use Over-the-Ear Headphones: Opt for larger headphones that rest over the ears instead of earbuds that go directly into the ear canal.
- Take Breaks: Give your ears regular breaks from headphone use to reduce exposure to loud noise.
- Routine Checkups: Get periodic checkups for your ears to monitor any signs of potential hearing loss.
Treatment and Diagnosis
If you suspect hearing loss, it is essential to consult a healthcare professional. A doctor may conduct a physical examination of your ears and recommend further tests like audiometry or tuning fork tests. While some types of hearing loss are irreversible, early diagnosis can help manage and mitigate its effects on your quality of life.
Hearing Impairment in Australia
In Australia, it was estimated that 3.55 million Australians had hearing impairment in 2005. By 2010, the number of Australians with hearing impairment was projected to increase to 4.02 million.
The prevalence of hearing impairment varies across different age groups and demographics.
Hearing Impairment in Adults:
- One in six Australians is affected by hearing impairment.
- Men have a higher incidence of hearing impairment than women.
- The most common causes of hearing impairment/loss in adults are aging and excessive exposure to loud sounds.
- Over 50% of the population aged between 60 and 70 years experience some form of hearing impairment.
These statistics highlight the significant impact of hearing impairment on the Australian population across different age groups and demographics.
